What kind of toothpaste do you like to use? This hygienist is actually a Crest person. Everyone has their certain brand, but Colgate Total is the number one recommended by dental professionals. Colgate Total helps prevent and treat gingivitis. Colgate Total has been researched and tested in depth more than any other brands of toothpaste worldwide. In fact, it is one of the few toothpastes that is approved by the FDA (Food & Drug Association).
People have started to panic due to reports that the ingredient Triclosan contained in Colgate Total is linked to cancer cell growth. Some questions about triclosan’s impact on people cannot be answered. People are exposed to many chemicals that may interact in the body which makes it hard to link one substance to one disease. Colgate Total has been on the market for almost eighteen years, and there has been no sign of a safety issue.
Colgate Total is approved by the ADA and more than forty dental associations. Agencies in the United States, Australia, and Europe have performed their own studies of Colgate Total, and all of them have confirmed that it is safe and effective in fighting and reversing gingivitis. It is the only triclosan toothpaste approved to be sold in the United States. If you have any questions, feel free to ask a member of our dental team!








 To help your children stop this habit, try to encourage them with rewards. Provide them with a toy after a certain amount of days they go without sucking their thumb. Mark progress on a calendar where the child can see the progress he/she is making. Most important, no nagging! Children get defensive if the parent is nagging to much about stopping the habit.
To help your children stop this habit, try to encourage them with rewards. Provide them with a toy after a certain amount of days they go without sucking their thumb. Mark progress on a calendar where the child can see the progress he/she is making. Most important, no nagging! Children get defensive if the parent is nagging to much about stopping the habit. they are burning. Sometimes the burning sensation can affect the whole mouth, and not just a certain area. Although Burning Mouth Syndrome can affect anyone, it is most common in middle-aged or older women.
they are burning. Sometimes the burning sensation can affect the whole mouth, and not just a certain area. Although Burning Mouth Syndrome can affect anyone, it is most common in middle-aged or older women. Depending on the cause of BMS, there are medications that can be prescribed to treat the oral candidacies, anxiety, and depression. There are also prescriptions and supplements to relieve dry mouth. Biotene mouth wash is commonly used to treat dry mouth. At home treatment can include sucking on ice chips, drinking plenty of water, avoiding hot and spicy foods, avoiding acidic foods and drinks, and avoiding alcohol and tobacco. If you have any questions about Burning Mouth Syndrome, call our office or physician for more information.
Depending on the cause of BMS, there are medications that can be prescribed to treat the oral candidacies, anxiety, and depression. There are also prescriptions and supplements to relieve dry mouth. Biotene mouth wash is commonly used to treat dry mouth. At home treatment can include sucking on ice chips, drinking plenty of water, avoiding hot and spicy foods, avoiding acidic foods and drinks, and avoiding alcohol and tobacco. If you have any questions about Burning Mouth Syndrome, call our office or physician for more information. The purpose of sealants is to prevent cavities. We recommend children as well as adults to have sealants. As soon as the 6 year molars have fully erupted on your children, you should consider having sealants placed. The 6 year molars (first molars) usually come in between ages 5-7, but that can vary. Later when the 12 year molars erupt, those can also be sealed. The 12 year molars (second molars) usually erupt between ages 8 ½ to 13 years old. Besides, children, anyone who is prone to get cavities should consider getting sealants. Also anyone with deep groves in the biting surfaces of their teeth should consider sealants, since they are hard to keep clean.
The purpose of sealants is to prevent cavities. We recommend children as well as adults to have sealants. As soon as the 6 year molars have fully erupted on your children, you should consider having sealants placed. The 6 year molars (first molars) usually come in between ages 5-7, but that can vary. Later when the 12 year molars erupt, those can also be sealed. The 12 year molars (second molars) usually erupt between ages 8 ½ to 13 years old. Besides, children, anyone who is prone to get cavities should consider getting sealants. Also anyone with deep groves in the biting surfaces of their teeth should consider sealants, since they are hard to keep clean.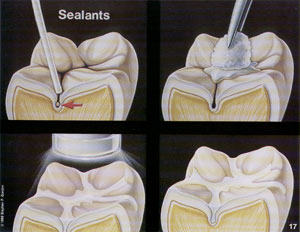 To place a sealant, the tooth must be very dry. Any kind of moisture could prevent the sealant from adhering to the tooth. To ensure dryness, cotton rolls may be placed around your tooth. Next a preparation gel called etch is placed on the tooth. Then that gel will be washed and suctioned (vacuumed) off and the tooth dried by blowing air. Next a bonding agent will be “painted” on the tooth. Then a blue colored ultraviolet (u.v.) light is used to activate the bonding agent. Then the sealant is placed in the groves of the biting surfaces of the tooth. Finally the blue u.v. light is used to make the sealant harden. You may be asked to close your eyes or wear orange colored glasses because it is not good for your eyes to stare at the blue u.v. light.
To place a sealant, the tooth must be very dry. Any kind of moisture could prevent the sealant from adhering to the tooth. To ensure dryness, cotton rolls may be placed around your tooth. Next a preparation gel called etch is placed on the tooth. Then that gel will be washed and suctioned (vacuumed) off and the tooth dried by blowing air. Next a bonding agent will be “painted” on the tooth. Then a blue colored ultraviolet (u.v.) light is used to activate the bonding agent. Then the sealant is placed in the groves of the biting surfaces of the tooth. Finally the blue u.v. light is used to make the sealant harden. You may be asked to close your eyes or wear orange colored glasses because it is not good for your eyes to stare at the blue u.v. light.